Background
Chronic lymphocytic leukemia (CLL) is a disease of the elderly. Advancing age is associated with greater vulnerability, increasing treatment side effects and reduced survival with chemoimmunotherapy (CIT). Comorbidities burden, Charlson Comorbidity Index (CCI) and Cumulative Illness Rating Scale (CIRS) scores emerged as reliable tools in trials with patients (pts) receiving CIT. Ibrutinib changed CLL treatment paradigm. Nevertheless, adverse events leading to dose reductions and discontinuations are frequent in everyday practice. Finally, it is still unclear whether age, ECOG and comorbidities retain a predictive value with ibrutinib and if number and types of concomitant medications may interfere with treatment outcome.
Methods
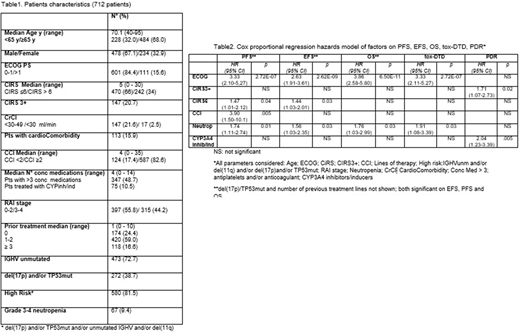
This multicenter retrospective analysis evaluated 712 pts in 15 Italian centers treated with ibrutinib from March 2014 to May 2020. We analyzed the impact of age (<65y, vs ≥ 65y) , CIRS (≤6 vs >6), major CIRS comorbidity (at least one organ with a CIRS score ≥3, CIRS3+), ECOG (0-1 vs >1) and CCI (<2 vs ≥2) in definitive treatment discontinuation due to toxicity (tox-DTD); permanent dose reduction (PDR); EFS (definitive treatment discontinuation for any reason, progression, death); PFS and OS. Medical conditions that were deemed to be CLL complications and CLL diagnosis, were not included in CIRS calculation.
Survival functions for the time-to-event variables were estimated by Kaplan-Meier method and related strata compared using the log-rank test. Multivariate analyses were also performed using the Cox regression.
Results
Table 1 shows pts characteristics. Median follow-up was 26.6 months (range 3 - 75.8); median months on ibrutinib, 21.2 (range 3 - 75.4). Overall, 440 (61.8%) pts are continuing treatment. A total of 272 pts (38.2%) permanently discontinued ibrutinib: 128 (18%) due to toxicity; 132 (18.5%) due to progressive disease/Richter Transformation; 13 (1.8%) for other reasons. Of 712 pts, 325 (45.6%) discontinued treatment for ≥7 days with a median of 15 days/pts interruption. At least one dose reduction occurred in 219 pts (30.8%) and in 123 (17.3%) ibrutinib was permanently administered at a lower dosage. Toxicity was the main reason for PDR (175 pts). Concomitant medications were recorded in 624 (87.6%) pts, 374 of whom took ≥4 drugs in addition to ibrutinib. In 75 cases ibrutinib was concomitant with CYP3A4 inhibitors/inducers. At univariate analysis age ≥ 65y, CIRS>6, CIRS3+, ECOG >1 and CCI ≥2, showed to be significant for tox-DTD. All parameters except age ≥ 65y had an impact on PDR. ECOG >1 was the only parameter affecting PFS, EFS and OS (p<.0001), while CIRS>6 negatively influenced PFS and EFS but not OS. In pts stratification according to age, only in the elderly CIRS >6 was significant for tox-DTD (p 0.009), PDR (p<.0001), PFS (p 0.022) and EFS (p .0002). CIRS3+ instead, was associated to tox-DTD and PDR both in the younger (p .0002 and p .0182, respectively) and older population (p .0128 and p 0.011, respectively). While CIRS3+ did not influence outcome in the younger, it determined a shorter EFS in the elderly. At the Cox regression analysis, ECOG >1 and CIRS>6 were the only fitness-related parameters affecting both PFS and EFS; the influence of ECOG was significant for tox-DTD and OS also (Table 2). CCI ≥2 had an impact on PDR only. Baseline neutropenia also influenced pts tox-DTD and all survival outcomes. Treatment with CYP3A4 inhibitors/inducers was independently associated with higher PDR. Pts outcome in terms of EFS, PFS and OS was also significantly dependent on number of previous lines of treatment (0 vs 1-2 vs ≥3) and presence of del17p/TP53 mutation (not shown in table 2). Ibrutinib PDR did not affect PFS and OS, while OS was significantly reduced in pts definitively discontinuing treatment due to toxicity (p <.0001).
Conclusions
To our knowledge this is the largest series analyzing the role of age, comorbidities and concomitant medications in pts treated with ibrutinib. In univariate analysis the incidence of tox-DTD and PDR was significantly higher in pts with CIRS3+ and in elderly pts with CIRS>6. ECOG>1 significantly affected pts outcome. Furthermore, CIRS>6 was associated with shorter EFS and PFS in elderly. In the Cox regression hazards model ECOG and CIRS>6 were the only fitness-related factors influencing outcome. Baseline neutropenia also emerged as a parameter significantly affecting both treatment management and survival outcomes.
Tedeschi:Abbvie: Honoraria, Speakers Bureau; Acerta: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Beigene: Honoraria, Speakers Bureau; Sunesis: Honoraria, Speakers Bureau. Coscia:Karyopharm Therapeutics: Research Funding; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Shire: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Ciolli:Abbvie: Research Funding; Janssen: Honoraria. Reda:Abbvie: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees. Laurenti:Janssen: Honoraria; Gilead: Honoraria; AbbVie: Honoraria; Roche: Honoraria. Varettoni:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel/accommodations/expenses; Roche: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Other: Travel/accommodations/expenses. Murru:Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Sportoletti:AbbVie: Honoraria; Janssen: Honoraria. Vitale:Janssen: Honoraria. Di Raimondo:Takeda: Consultancy, Honoraria; GSK: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Amgen, Takeda, Novartis: Honoraria; GILEAD, Incyte: Research Funding. Montillo:F. Hoffmann-La Roche: Honoraria, Research Funding; AbbVie: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Astra Zeneca: Honoraria; Gilead: Honoraria, Speakers Bureau; Verastem: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal